Renal Function Tests( RFTs) provide crucial details regarding the condition of your kidneys. Kidneys are like filtration machine for your body. Urine is produced by kidneys, which also filter waste from the blood. Numerous chemicals in the blood are controlled by the kidneys. Your kidneys aid in blood pressure regulation.
The kidneys produce a variety of compounds, urine being just one of them. Your kidneys are crucial organs that carry out a variety of tasks to keep your blood clean, free of toxins, and correctly balanced .Typically, a person has two kidneys. Each kidney in your body is a bean-shaped organ around the size of your fist. They are situated directly below the ribs in the center of your back. Your kidneys process 200 Liters of blood per day, removing around 2 Liters of waste and surplus water in the process. The kidneys also control extracellular fluid volume, serum osmolality, and electrolyte concentrations.
How do the Kidneys function?
*Control blood molecules including salt, potassium, calcium, and phosphorus as well as bodily water.
*Create a urine filter and discard waste.
* 3 Important Hormones are released to help in the following processes:
1.Keeps your blood pressure under control
2.Maintains the health of your bones.
3. Encourage the production of red blood cells by the bone marrow.
Three Important Hormones produced by the kidneys:
1.Erythropoietin , which increases the creation of red blood cells in the bone marrow,
2.Renin, which regulates blood pressure.
3.Calcitriol(1,25-dihydroxyvitamin D) , also known as vitamin D’s active form , supports the body’s proper chemical balance as well as the maintenance of calcium for strong bones.
What are Renal Function tests(RFTs) and their Significance?
This article provides an update on the relevant biochemical assays for assessing renal function.
Renal Function Tests – Video / Animation
Sample Collection
Assessment of Renal Function Tests

Glomerular Filtration Rate ( GFR)
It must pass through an unrestricted filter at the glomerulus.
It cannot be either reabsorbed or released by the renal tubule. It shouldn’t be gotten rid of outside the body. Because there isn’t an endogenous marker for GFR yet, exogenous indicators are used.
Stages of Chronic Kidney Disease
Stage 1 with normal or high GFR (GFR > 90 mL/min)
Stage 2 Mild CKD (GFR = 60-89 mL/min)
Stage 3A Moderate CKD (GFR = 45-59 mL/min)
Stage 3B Moderate CKD (GFR = 30-44 mL/min)
Stage 4 Severe CKD (GFR = 15-29 mL/min)
Stage 5 End Stage CKD (GFR <15 mL/min)
Serum Creatinine Test
Serum creatinine is a byproduct of muscle metabolism. It is removed from the blood by the kidneys and subsequently excreted in the urine. The serum creatinine test measures the amount of creatinine in the blood. Elevated creatinine levels can be a marker of impaired kidney function because healthy kidneys should be able to filter creatinine from the bloodstream adequately.
Reduced renal clearance leads to an increase in blood creatinine. Muscle mass has an impact on creatinine generation on a daily basis. As a result, males and females with lower creatinine readings in children and those with less muscle mass have different creatinine ranges.
Diet can also affect creatinine levels. Consuming red meat can affect creatinine levels by 30%. It is possible to determine the glomerular filtration rate (GFR), a significant indicator of kidney function, with the help of this simple and often used test.
The computed creatinine clearance serves as a gauge of GFR. It is important to collect urine over a period of 24 hours, or preferable during a precisely scheduled period of 5 to 8 hours, because 24-hour collections are infamously unreliable. The creatinine clearance is then calculated using the following equation:
C = (U x V) / P
Clearance is represented by U = urine concentration,
V = urinary flow rate (volume/time, i.e. ml/min), and P = plasma concentration.
Blood urea nitrogen, or BUN Testing
The blood urea nitrogen test (BUN) measures the urea nitrogen content of the blood. Urea is created as a waste product when the body breaks down proteins. Urea, also referred to as BUN, is a nitrogen-containing molecule that is created in the liver as a byproduct of protein metabolism in the urea cycle.
Because the kidneys remove urea from the bloodstream, elevated BUN levels may be a symptom of renal illness. But it’s crucial to keep in mind that other factors, like diet, dehydration, and some medications, can also affect BUN levels. Therefore, BUN results should be viewed in the context of other renal function tests.
Around 85% of the urea is excreted via the kidneys, with the remaining urea being passed through the GI tract In acute and chronic renal failure/impairment Serum urea levels increases when renal clearance decreases. Other conditions that might produce a spike in urea include upper GI bleeding, dehydration, catabolic states, and high-protein diets that are unrelated to renal diseases. It is possible for urea synthesis to be decreased in famine, low-protein diets, and severe liver diseases. Although serum creatinine is a more accurate indicator of renal function, urea is raised earlier in renal disease.
When the BUN is elevated, the ratio of BUN to creatinine can be used to distinguish between pre-renal and renal causes. The ratio is similar to 20:1 in pre-renal disease, while it is similar to 10:1 in intrinsic renal disease. A BUN to creatinine ratio that is extremely high (often greater than 30:1) has been linked to upper GI hemorrhage.
Cystatin C
All nucleated cells in the body create cystatin C, a low-molecular-weight protein that serves as a protease inhibitor. which is freely filtered by the glomeruli (small filters in the kidneys). The cystatin C test is an alternate marker for calculating GFR that analyzes the amount of cystatin C in the blood. It is more effective in some clinical conditions than creatinine since it is less affected by muscle mass and diet.
Glomerular filtration rate (GFR) and serum levels of cystatin C are inversely correlated. In other words, high values for creatinine and low values for GFRs both imply low GFRs. Contrary to creatinine, cystatin C is processed differently by the kidneys. Cystatin C must first be filtered before it can be reabsorbed and digested by the proximal renal tubules, in contrast to creatinine, which can be freely filtered by both glomeruli.
Therefore, under typical circumstances, cystatin C does not significantly permeate the final urine void. Serum and urine are both used to measure cystatin C. Cystatin C has several advantages over creatinine, including the fact that it is unaffected by age, muscle mass, or nutrition, and that it is a more accurate indicator of GFR than creatinine, particularly in the early stages of renal impairment. The presence of cancer, thyroid disease, and smoking can all affect cystatin C levels.
Urine analysis
Albuminuria and Proteinuria
Albuminuria is the medical term for the abnormal accumulation of albumin in the urine. The term “microalbumin” is now solely used to refer to urine albumin because there is no such biological molecule as microalbumin. Albuminuria in diabetics is a symptom of nephropathy in its early stages. It implies increased endothelial permeability and is a marker for chronic renal impairment as well as a stand-alone predictor of cardiovascular disease.
When analyzing 24-hour urine collections or a random or early-morning sample, urine albumin can be calculated as an albumin/creatinine ratio. When a urinary tract infection has been ruled out and albuminuria has appeared twice, glomerular dysfunction is the most likely explanation. A three-month or longer period of albuminuria indicates chronic renal dysfunction. Frank proteinuria is defined as consuming more than 300 mg of protein per day. A typical urine sample may include up to 150 mg of protein per day (30% albumin, 30% globulins, and 40% Tamm Horsfall protein).
Protein levels in the urine could rise as a result of: Glomerular proteinuria is caused by conditions that impair the glomerular filtration barrier’s ability to permanently select for plasma proteins, like glomerulonephritis or the nephrotic syndrome.
Tubular proteinuria, which results from inadequate tubular protein reabsorption (for instance, in interstitial nephritis), Increased blood levels of proteins (such myoglobinuria and the multiple myeloma-Bence Jones protein) cause overflow proteinuria .urogenital tract cancer or inflammation. Urine protein can be assessed using a 24-hour urine collection or a random urine protein-to-creatinine ratio; an early morning sample is favored because it is almost representative of the 24-hour sample.
The KDIGO classification distinguishes three albuminuria stages:
A1: fewer than 30 mg/g of creatinine
A2: 30 to 300 mg/g of creatinine.
A3: Exceeds a creatinine level of 300 mg/g
Nephrotic syndrome is characterized by a daily excretion of 3.5 g of urine protein and is associated with edema, hypoalbuminemia, and hypercholesterolemia.
Tests of Renal Tubular Function
The ability of the renal tubules, which are in charge of the reabsorption and secretion of numerous chemicals in the kidneys, to operate is determined in part by the results of tests for kidney tubular functions. Conditions include kidney illnesses, electrolyte imbalances, and metabolic disorders that impact tubular function can be diagnosed and monitored with the aid of these tests.
The following are some typical tests to evaluate kidney tubular functions:
pH of Urine: This test determines whether urine is acidic or alkaline. Tubular dysfunction may be indicated by abnormal pH levels.
The Urine Specific gravity test determines the amount of solutes present in the urine. It can be used to evaluate how well the kidneys concentrate urine.
The Urine Osmolality test provides more precise information on the kidney’s capacity to concentrate urine by measuring the concentration of solutes in urine.
Testing for Renal Tubular Acidosis (RTA): RTA is a term used to describe a group of illnesses that compromise the kidney’s capacity to eliminate acid appropriately. The pH of the urine, bicarbonate levels, and blood may all be measured during these examinations.
Test for Glucose Tolerance: In some cases, tubular malfunction can cause glucose to show up in the urine (glucosuria). This condition can be detected with the aid of a glucose tolerance test.
Testing for Aminoaciduria: This procedure looks for amino acids in the urine. Aminoaciduria may indicate metabolic issues or dysfunction of the renal tubules.
Test to Measure Phosphate Reabsorption: This test measures the kidney’s capacity to reabsorb phosphate. It is utilized to assess how well the renal tubules handle phosphate.
The Urine Urea Nitrogen Test(UUN), measures the amount of urea nitrogen present in the urine and evaluates the kidney’s capacity to reabsorb urea.
Creatinine clearance in the urine can give information on overall kidney function, which includes tubular function, even if it is not specific to tubular function. In order to measure the glomerular filtration rate (GFR) and determine how much creatinine is removed by the kidneys, urine and blood samples must be taken.

Indications of Renal Function Tests:
Renal function tests are used to evaluate the condition and efficiency of the kidneys. Healthcare professionals request these tests for a variety of reasons, including to detect kidney illnesses, track kidney function, and assess general health.
The following are some typical causes for requesting renal function tests:
Renal function tests are frequently included in standard health examinations, particularly for people who have risk factors such diabetes, hypertension, a family history of kidney disease, or a history of renal issues. Regular testing can aid in early detection of renal problems.
Renal function tests are primarily carried out to diagnose renal disease, choose the best patient care strategy, and prevent further decline in renal function. When a known or potentially nephrotoxic treatment drug is started for patient management, renal function tests may be necessary to assess and monitor renal function.
In order to determine whether transplant recipients are initially suitable as donors and to keep track of any major decline in renal function following the donation, renal function tests are also indicated.
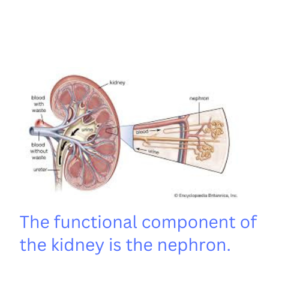
Renal function tests can also be used to determine whether a particular element of the nephron, the kidney’s functional unit, is compromised, such as glomerular vs tubular disease.
Analyzing urine amino acids, glucose, phosphate, and pH during renal function testing can help identify tubular function issues such as Fanconi syndrome.
Renal function tests are necessary on a frequent basis for people who have been diagnosed with chronic kidney disease (CKD) in order to track the disease’s development. These examinations aid in assessing the degree of kidney impairment and informing therapy choices.
Assessing Kidney Function Before Surgery: The kidneys may be under stress during some operations or medical procedures, particularly those that use contrast agents. Before these treatments, healthcare professionals may perform renal function tests to evaluate kidney function and make sure the kidneys can handle the added load.
Analyzing Dehydration: Renal function tests, such as blood urea nitrogen (BUN) and serum creatinine, can assist diagnose kidney impairment brought on by dehydration. Dehydration can impact kidney function.
Urine analysis and renal function tests can both help in the diagnosis and follow-up of kidney stones. Elevated blood levels of chemicals like calcium, oxalate, or uric acid may signify a propensity for the development of stones.
Urinalysis, a component of renal function testing, can detect urinary tract infections (UTIs) by looking for white blood cells, red blood cells, or bacteria in the urine. If a UTI is not treated, it may occasionally result in kidney infections.
Evaluating Medication Effects: Certain medications, including some pain relievers and antibiotics, can affect kidney function. Healthcare providers may order renal function tests to monitor the impact of medications on the kidneys, especially when using them long-term or at higher doses.
Proteinuria: Proteinuria, or the presence of excess protein in the urine, can be a sign of various kidney diseases, such as glomerulonephritis or nephrotic syndrome. Renal function tests, particularly urine protein tests, can help diagnose and monitor these conditions.
Monitoring Autoimmune Disorders: Autoimmune diseases like lupus and vasculitis can affect kidney function. Renal function tests help assess kidney involvement and guide treatment decisions.
Analyzing Electrolyte Balance: The kidneys are essential for preserving the body’s electrolyte balance. Electrolyte imbalances, including those involving potassium, sodium, and calcium, can be found using renal function testing.
It’s crucial to speak with a healthcare professional to decide which kidney function tests are most appropriate for you given your medical history, symptoms, and risk factors. Early identification and monitoring of kidney-related problems can result in prompt therapies and better renal health outcomes.

Complications
Renal function tests can have difficulties or have other restrictions, despite the fact that they are often safe and well-tolerated. Here are some potential issues and things to think about: With the exception of those involving venipuncture, complications with the bulk of renal function tests are uncommon.
The danger of infection at the location of the blood draw is minimal, however it does occur sometimes. This risk is reduced with the implementation of proper sterile procedures.
Allergic Reactions: Although rare, allergic reactions to the compounds used in renal function testing, such as contrast agents in some imaging examinations, are possible in some people. If you have a history of allergies, let your doctor know.
Contrast-Induced Nephropathy (CIN): Contrast chemicals used in imaging examinations like CT scans or angiograms can occasionally have an impact on kidney function, especially in people who already have kidney issues. Before utilizing contrast agents, healthcare professionals should consider the risk of CIN.
False Results: The outcomes of renal function tests can be impacted by a number of variables, including dehydration, recently intense activity, specific drugs, and food. To get accurate findings, it’s crucial to adhere to any pre-test instructions given by your healthcare professional. Patients should also be instructed to continue drinking water on a regular basis before these assessments.
Emotional Stress: Some patients may experience stress or worry as a result of the testing procedure, which may momentarily impair kidney and blood pressure function. When analyzing results, healthcare professionals should be mindful of these aspects.
Radiation Exposure: Ionizing radiation, which presents a tiny risk of injury, is exposed during several imaging tests, such as CT scans. When these tests are required by medicine, the advantages typically outweigh the hazards.
Kidney harm: The use of various drugs or contrast agents for diagnostic reasons may occasionally result in transient kidney harm. Healthcare professionals usually have the ability to reverse this and continuously monitor you.
Conclusion
Renal function tests are essential instruments for evaluating kidney health and identifying renal diseases. The course of kidney disease and its complications can be stopped by early detection and monitoring of renal dysfunction. Regular renal function testing is crucial if you have kidney disease risk factors like diabetes, hypertension, or a family history of kidney issues. Based on your particular risk factors and health status, speak with your healthcare practitioner to decide on the right tests and how frequently to get them done. Keep in mind that prompt action can greatly enhance the prospects for kidney health and general wellbeing.